February 2023
Preparing for Weight Loss Surgery & The Liquid Diet Stage

If you've been considering Weight Loss Surgery, you most likely have questions about how to prepare and what the recovery process will likely look like. Your professional team will be the first line of advice, but it's important to be well-read on all things bariatric so you are well-prepared mentally and physically every step of the way.
Weight Loss Surgery (also called Bariatric Surgery) can be both an exciting and overwhelming experience. Before embarking on this new chapter of your life, it's important to understand how it impacts your ability to eat and absorb food and how it will ultimately change your dietary patterns before and after surgery.
Three types of Weight Loss Surgeries are routinely performed: gastric band, gastric sleeve and gastric bypass. The gastric band (or lap band) is a silicone band that attaches around the top part of the stomach, creating a smaller pouch and helping you feel full on a small amount of food. This surgery is not commonly performed anymore and is the only reversible Weight Loss Surgery.
Gastric sleeve is the most common of the three procedures, accounting for around 60% of the Weight Loss Surgeries performed. In Gastric Sleeve Surgery, the surgeon makes a sleeve or banana-shaped pouch out of the stomach and removes around 70-80% of its capacity, impacting how much food you require before feeling full.
Gastric Sleeve Surgery is also referred to as Metabolic Surgery, as removing this part of the stomach has far-reaching hormonal effects on "hunger hormones" ghrelin, adiponectin and insulin. Alongside reduced capacity, patients also welcome some relief from the eternal feeling of hunger for 12-18 months after the procedure.

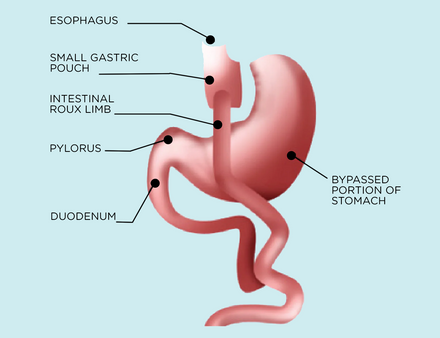
Gastric bypass (also called the Roux-en-Y) makes up around a third of weight loss surgeries. In Gastric Bypass Surgery, a small section on the top of the stomach is connected directly to the second section of the intestine (the jejunum), bypassing the first section (the duodenum).
Similarly to the sleeve and band, the bypass restricts the size of the stomach, limiting how much food you can eat at once. However, the bypass has increased limits on how well food can be absorbed.
Regardless of which surgery you and your surgeon decide on, how you eat before and after the operation will greatly impact how well you recover and how likely you are to maintain a healthy weight in the following years.
The Bariatric Surgery diet phases are broken down into five phases:
- Phase 1: Pre-operative Diet Phase
- Phase 2: Post-operative Clear Fluid Phase
- Phase 3: Post-operative Full Fluid Phase
- Phase 4: Pureed Food Phase
- Phase 5: Soft Food Phase
- Phase 6: Normal Food Phase
When using the term 'diet' in this blog, we're referring to the food you'll be eating daily. Although there will be guidelines on how to eat post-surgery for the best outcomes, it's important to know that there isn't a strict 'diet' you'll need to follow once you have worked through the texture stages and recovery process.
You will just have certain "rules" to follow to help ensure your success. We will cover these in future articles.
In this article, we'll discuss the first three phases and give you tips to ensure you're making the most of your nutrition during each one.
Phase 1: The First Steps
Along with doctors' visits, evaluations and decisions around which surgery to have, you may also have meetings with a dietitian to discuss how the way you eat will change throughout the surgery preparation and recovery process.
The first dietary change will occur when you commence your pre-operative diet, also called the pre-op liquid phase, VLED (very low energy diet) or VLCD (very low calorie diet.) This 'diet', or phase, usually starts 2 – 4 weeks before surgery. During this stage, meal replacement shakes to replace all or some of the nutrition your body would usually receive from food.

Generally, that means either 2 shakes daily, a healthy meal or 3 shakes daily, providing around 2400kJ (600kcal) and all the protein, vitamins and minerals needed. Your team always determines this - even if your friend did it somehow differently, you need to stick to your plan because it will be laid out for your safety during the surgical procedure.
In addition to these shakes, you might be allowed 2 cups of approved, low-carbohydrate vegetables and calorie-free drinks such as water, diet soft drinks, tea or coffee (without milk).
The main purpose of the pre-op stage is to help the liver break down its stored sugar (glycogen) and put the body in a mild ketosis state. This helps reduce the liver's size and makes it easier for the surgeon to manoeuvre during keyhole surgery.
Your safety and the procedure's success must ensure you follow your pre-operative diet carefully and do not have any food or drinks that your doctor or dietitian has approved.

How to choose a shake?
There are countless meal replacement shakes on the market, and knowing which one to choose is likely the first challenge you'll face when starting your pre-op diet. Unfortunately, not all meal replacement shakes are made equal, so it's worth researching and finding the one that will give you the best outcome and chance at surgery success.
So, what does that look like exactly? There are a few key considerations when choosing a pre-op liquid diet shake. The best shakes on the market are those that:
- Specifically, state they are suitable for the 'VLCD' - (very low-calorie diet) or 'VLED' (very low energy diet)
- Can be made on water instead of requiring milk: - A good meal replacement shake will contain all of the micronutrients your body needs throughout the day and will not require the addition of milk. If a meal replacement shake asks to add in milk, it likely does not contain everything your body needs and should be avoided during your pre-surgery diet phase.
- Prioritise protein. The protein in your meal replacement shake will help keep you full and aid immune function and muscle retention. Choose a shake with around 30g of protein per serve.
- They are low in carbohydrates and fat. The purpose of the pre-operative liquid diet is to remove stored sugar and fat from your liver. Choose a shake that is low in both of these nutrients for the best results.
- Benefit your gut health. Whilst not essential, the best meal replacement shakes have added fibre and probiotics to help support your gut health. They should also not use artificial colourings and flavours, which may act as a gut irritant. Fibre and probiotics help feed and support your microbiome, which is important for your immune system and potentially a quicker recovery.
Our BN Slim has all the above features whilst also being gluten-free, low-GI and tasting delicious!
Phase 2: Straight Out of Surgery
So, you've finished the preoperative diet phase and had the surgery; now what? The first step in the recovery process is to start on a clear fluids diet.
This diet is followed immediately post-op and usually lasts only a few days.
The purpose of this diet is to help keep you hydrated whilst minimising any gut and stomach irritation on the fresh surgical site. During the clear fluids stage, you'll be allowed to drink see-through non-carbonated drinks such as water, broth, tea (without milk), flavoured protein water, dilute juices and cordials, or any clear fluid that you may be able to add tasteless protein too.

Phase 3: More Liquids Again?
The next phase of your recovery will be moving onto free fluids or the full liquid diet phase. As daunting as this may sound, you can sigh relief that the worst liquid phases have ended! This phase is recommended for at least 2 weeks after your surgery; however, it will depend on your recovery progress.
The full-liquid phase includes any fluids that are smooth, lump-free and thin enough to run through a straw. As with the clear fluids diet, the full-fluid diet is also used to minimise any irritation to your gut during its healing process and reduce the strain placed on the stomach.

During this time, it's important to avoid carbonated drinks, alcohol, and fluids with high amounts of sugar (no more than 15g per serve) or fat, as they may cause dumping syndrome.
So, we've covered what you can't eat, but what can you eat?
During this diet phase, prioritising your protein intake is essential! After surgery, your stomach can only hold a shot glass worth of food, so your intake will decrease dramatically. During this time, however, your body needs even more protein than usual to aid the recovery and healing process of your muscle and skin cells.
A diet higher in protein will also help increase fat loss and reduce muscle loss, which is the exact goal of Weight Loss Surgery. Post-surgery, you must begin on your specific bariatric vitamins, which you will most likely need to take for the rest of your life.
Meal replacement shakes are still a great option, and the BN Slim Meal Replacement Shakes can also be used during this post-operative phase. However, if you're becoming bored of shakes, it can help to mix your diet up a little during this phase.
Some high-protein liquid diet ideas might include:
- Buying different flavours of shakes (The BN Slim comes in 3 yummy flavours to choose from).
- Making a milkshake with yoghurt, milk, blended fruit and added protein powder.
- Making a soup or broth with added bone broth powder increases the protein content.
- Mashed potato (thinned to a soupy consistency) with the added milk powder or neutral collagen powder.
Whilst there are plenty of liquid diet recipes online, investing in a bariatric-friendly cookbook at the start of your surgery journey can help build those healthy habits and stick to your diet phases through your recovery.
Phases 4 & 5: What's Next?
Once the liquid phases have been completed, your doctor will upgrade you to pureed foods for roughly 2 weeks, followed by soft foods for another two weeks (or as long as required for your safe recovery).
Pureed food should be smooth, lump-free and high in protein. You should introduce pureed foods slowly as tolerated, aiming to work your way up to 3 meals and 1 –2 snacks per day. It's important to keep your food moist, adding milk or water if needed and using a blender or food processor to get it to a smooth consistency.

Next, you'll move on to a soft-food diet stage. During this phase, foods will no longer need to be pureed. However, they should still be moist and soft enough to cut with a fork.
For both the liquid and soft food phases, you should continue to prioritise protein intake, aiming for at least 60g - 80g (1g of protein per kilogram of 'ideal" weight) per day. To do this, incorporate high-protein options such as meat, dairy, eggs, fish and legumes. You may also add protein powder or an instantised collagen powder to increase the protein content of your meals.
Although your doctor or dietitian will likely discuss healthy eating guidelines and portions post-surgery, there is no strict diet you will be required to follow after working through the texture phases. To ensure you're meeting all your nutrient requirements and maintaining your weight loss progress, it's important to be mindful of the types of foods and the amount you eat and drink for the rest of your life.
Part of this is also the incorporation of a Bariatric Multivitamin every day to support the restriction and malabsorption brought about by the surgery. Weight Loss Surgery is a great tool to help you achieve your health and weight goals.
However, it is only a tool, and your nutrition and exercise habits are essential for a healthy lifestyle and sustained weight loss.


